We’ve all felt puffed running to the bus, but shortness of breath doing every day activities may not be normal. Breathlessness, sometimes called dyspnoea, is an uncomfortable sensation of breathing discomfort. It can occur acutely or chronically.
There are lung, heart, blood, muscular and fitness causes of breathlessness. Sudden onset shortness of breath may be a medical emergency and require ambulance/ hospital admission to investigate for causes including pneumonia, collapsed lung (pneumothorax), asthma attack, fluid in the lungs (pulmonary edema) and heart attack (myocardial infarction).
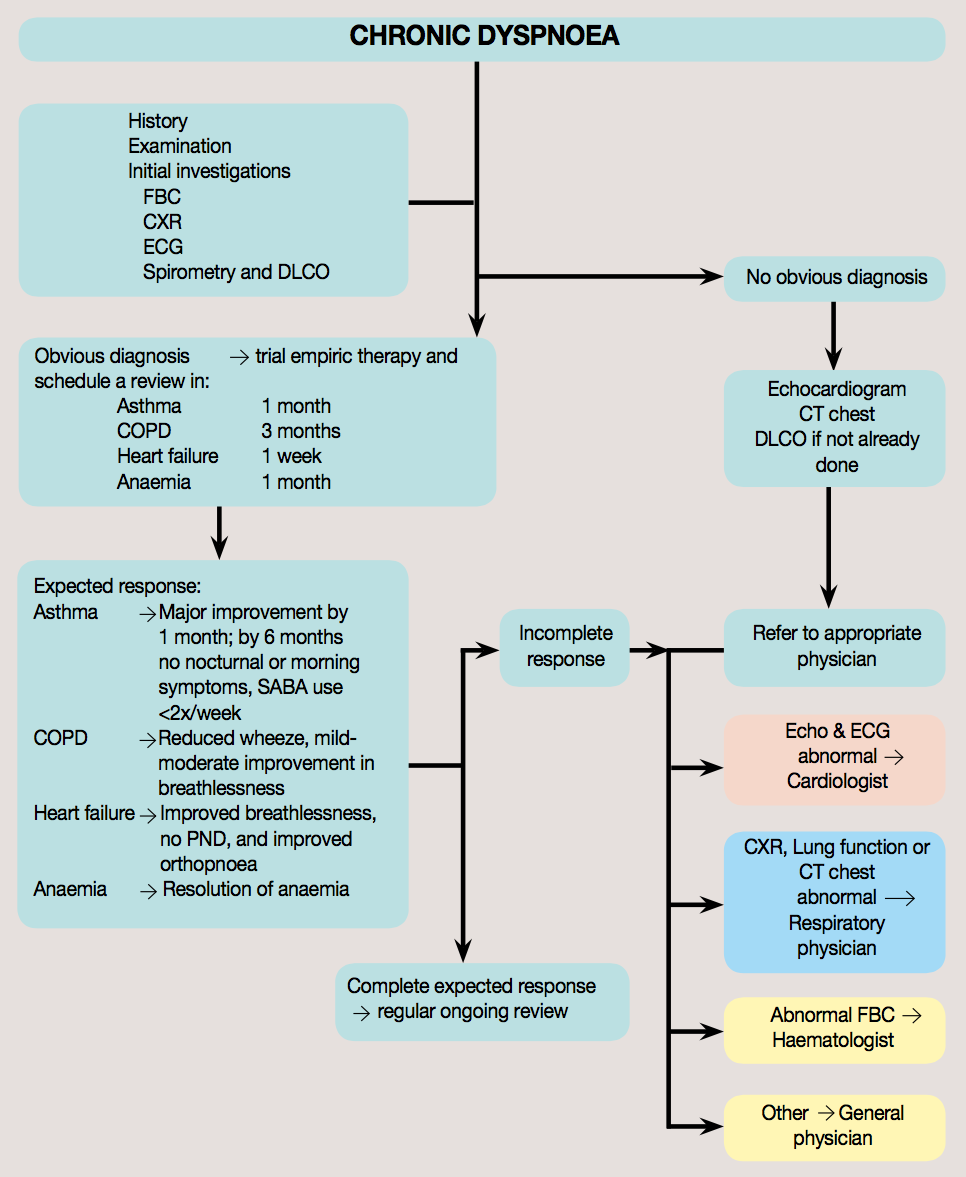
If you have shortness of breath develops and stays over weeks to months you should book in to see your GP for investigation and management to begin. Common lung causes include asthma and emphysema which are both conditions characterized by inability of the lungs to adequately empty air, sputum/phlegm production and wheeze.
The most common heart problem causing chronic shortness of breath is heart failure, a condition where damage to the heart causes inability to pump adequate blood around the body to meet demands. Other common causes that need investigating and ruling out are anemia and deconditioning.
My approach when seeing patients with chronic shortness of breath is to take a careful history regarding:
Duration of symptoms, what else was going on around the time the symptoms started
Severity of breathlessness - using either the "New York Heart Association" classification system or the "Medical Research Council" Dyspnoea score
Related symptoms e.g. chest pains, cough, sputum production
Pattern of symptoms e.g. Asthma is often worse around change of season, spring with exposures to pollen, winter and upper respiratory tract infections
Symptoms of heart failure e.g. waking up in the night gasping for breath, swelling in ankles
Possible causes of anaemia e.g. blood in bowel motions or heavy periods
Cigarette smoking history
Childhood history of lung infections
Any "Red Flag symptoms" e.g. coughing blood, chest pains
Past medical history and current medications are crucial pieces of the puzzle.
Examination and Investigations are both important and usually guided by the history that has been given. Ultimately once a differential diagnosis or working theory of what is going on has been formed, a trial of treatment is sometimes appropriate.
I think it is really important that if things are not getting better once a trial of treatment has been started, that other rarer causes, such as pulmonary hypertension be considered.